Cost Effectiveness Analysis (CEA)
What is Cost Effectiveness Analysis (CEA)
Cost-effectiveness analysis (CEA) is a decision-making tool that helps compare different ways to achieve a goal in terms of their resource utilization (cost) and outcomes (effectiveness). It can be used to find the cheapest way to achieve a goal, or to estimate the expected costs of achieving a particular outcome. It can also be used to compare the impacts and cost of various alternative means of achieving the same objective. The result of a CEA is expressed in a ratio (cost-effectiveness ratio, CER) between cost and outcome.
Understanding Cost Effectiveness Analysis (CEA)[1]
The best cost-effectiveness analyses take a broad view of costs and benefits, including indirect and longer-term effects, reflecting the interests of all stakeholders who will be affected by the program. So make sure the analysis is as comprehensive as possible.
The concept of cost-effectiveness is applied to the planning and management of many types of organized activity. It is widely used in many aspects of life. In the acquisition of military tanks, for example, competing designs are compared not only for a purchase price, but also for such factors as their operating radius, top speed, the rate of fire, armor protection, and caliber and armor penetration of their guns. If a tank’s performance in these areas is equal or even slightly inferior to its competitor, but substantially less expensive and easier to produce, military planners may select it as more cost effective than the competitor.
Cost-effectiveness analysis is not uniformly applied in the healthcare system. Decision makers often adopt new treatments without knowing if they are cost-effective. Even when cost-effectiveness has been studied, decision-makers may not be able to interpret the data, or they may not agree with the results. Despite this limitation, cost-effectiveness is increasingly used to inform healthcare decision makers.
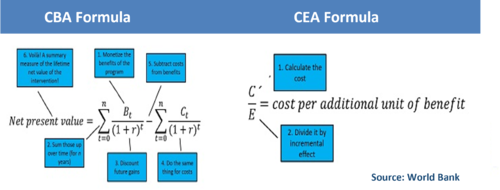
Cost-effectiveness analysis (CEA) considers alternatives in reference to the ratio between the costs associated with each alternative and a single quantified, but not monetary, effectiveness measure. This represents a complication of CEA as costs are represented by monetary values, while effectiveness may be measured in terms of saved lives, time savings or other similar quantifiable measures. For this reason, in CEA a ratio is calculated.
Explaining Cost Effectiveness Analysis (CEA)[2]
CEA is most useful when analysts face constraints which prevent them from conducting cost-benefit analysis. The most common constraint is the inability of analysts to monetize benefits. CEA is commonly used in healthcare, for example, where it is difficult to put a value on outcomes, but where outcomes themselves can be counted and compared, e.g. ‘the number of lives saved’.
CEA measures costs in a common monetary value (££) and the effectiveness of an option in terms of physical units. Because the two are incommensurable, they cannot be added or subtracted to obtain a single criterion measure. One can only compute the ratio of costs to effectiveness in the following ways:
CE ratio = C1/E1
EC ratio = E1/C1
where: C1 = the cost of option 1 (in £); and E1 = the effectiveness of option 1 (in physical units).
The first equation above represents the cost per unit of effectiveness (e.g. £s spent per life saved). Projects can be rank ordered by CE ratio from lowest to highest. The most cost-effective project has the lowest CE ratio. The second equation is the effectiveness per unit of cost (e.g. lives saved per £ spent). Projects should be ranked from highest to lowest EC ratios.
The outputs to be ranked by cost-effectiveness analysis will often be social or environmental in nature. For example, work in health economics looking at the cost-effectiveness of different treatments. As with CBA, the level of detail for the analysis will typically depend on the specific issue being addressed, but should take a broad view of costs and benefits to reflect all stakeholders.
Cost-effectiveness analysis (CEA) vs. Cost-benefit analysis (CBA)
There are a few key differences between cost-benefit analysis (CBA) and cost-effectiveness analysis (CEA). CBA measures the monetary value of all costs to all benefits, whereas CEA only calculates costs to outcomes of interest. This means that CBA is useful for making cross-comparative decisions across vastly different interventions (i.e., agriculture versus education), while CEA is used for comparing programs with common outcome(s) in mind, or when using nonmonetary values as well as monetary values are relevant to decision-making purposes.
CEA is more rigorous and in-depth than CBA, but it assumes a specific post-intervention trajectory. In contrast, CBA does not make any assumptions about the future and can be used for both pre- and post-intervention comparisons. Another important distinction is that while CBAs require a number of assumptions about the monetary values of all benefits, CEAs are transparent, simple and objective. Finally, while CBA measures the monetary value of all costs to all benefits, CEA only calculates costs to outcomes of interest.
While CBAs provide more information than CEAs about potential outcomes after an intervention, they are less able to calculate the cost of an intervention with respect to its benefits or effectiveness only. In contrast, CEAs are able to calculate the cost of an intervention with respect to its benefits or effectiveness only and can provide more detailed information about potential outcomes after an intervention.
When making decisions about which interventions to pursue, it is important to consider both CBA and CEA. However, given that CEAs are more rigorous and in-depth than CBAs, they should be used when there is a specific post-intervention trajectory in mind or when nonmonetary values as well as monetary values are relevant to decision-making purposes.
CBA calculates the monetary ratio of all costs to all benefits of a program. CBA can help to determine whether a program is worth the investment. It can also allow comparison across vastly different interventions (i.e. education versus agriculture). However, CBA requires a number of strong assumptions about the monetary value of all the different benefits, including the lifetime benefits of an intervention. In contrast, CEA is a transparent, simple, and objective measurement that enables comparison of programs with common outcome(s) of interest. However, the implicit assumption is a common post-intervention trajectory.
Considerations for cost calculations[3]
- Use program financial records. Typically, begin calculating costs by referring to program budgets, which provide a list of all relevant activities involved in implementing the program. Consider, however, that budgets are forward-looking estimates of true costs. Thus, it’s better to use actual program financial records on expenditures for calculations. However, this is not commonly done.
- Interview program and field staff to get key information including unit cost data like allocation of staff time across activities and wages for staff at various levels of implementation team. Note that using average wages makes calculations less sensitive.
- Model program costs at the margin. You want to capture marginal costs of new activities initiated as part of the interventions. For example, to calculate the costs of a school meals program, you may need the cost of new kitchen, cooks, implements, and food. However, you should not include the cost of school administration or buildings as these would exist whether or not the intervention was implemented.
- Consider depreciation. Account for how to value new assets or equipment obtained over the program implementation period.
- Consider the cost of user time. Include the costs of participation in program (i.e. using local wages).
- Differentiate between pilot costs and scale-up costs.
- Include spillover effects on indirect beneficiaries when quantifying impacts
Why Use Cost-Effectiveness Analysis?
There are many reasons why an organization might want to use cost-effectiveness analysis. Perhaps the most important reason is that it allows organizations to identify low-cost, high-impact interventions. For example, each year more than a million young children die from dehydration when they become ill with diarrhea. However, oral rehydration therapy is a way of treating diarrhea that does not diminish its severity or mortality rate. Oral rehydration therapy cost only $2-$4 per life year saved and was promoted by public policy to help save millions of lives worldwide .
Another reason for using cost-effectiveness analysis is that it helps identify where to allocate resources in order to maximize impact. A study at Harvard University focused on the 185 interventions which cost US$21 each year . This type of analysis can help countries make decisions about which interventions are most effective and allocation of funds.
Cost-effectiveness analysis is not always feasible, in which case spending might be directed towards more cost-effective interventions instead. However, if done correctly, this process can provide valuable insights into how best to allocate resources in order to achieve the greatest impact possible.
How to do Cost Effectiveness Analysis[4]
- Decide which outcome you will use for the comparison: The first step is to decide which outcome you will use to compare the activities. It needs to be the same outcome for both activities so you are comparing apples with apples. It also needs to be something you can measure accurately. For example, the number of toilets built, the number of small businesses set up, the number of trees planted, or the number of children who don’t drop out of school. Make sure you clearly define how the outcome is measured. For example, if it is the number of pregnant women attending antenatal care, then how many visits do they need to attend? What if they only attend some visits? Or don’t complete all the required steps? The outcome needs to be measured the same way every time.
- Measure the outcome: If you are comparing the cost effectiveness for two activities then you need to measure the outcome in question for both activities. Let’s continue with the antenatal visit example. Say you want to compare one-on-one outreach with mass SMS messages. First you would need one group of pregnant women who don’t receive any intervention, and you would count how many of them attend antenatal care. For example, 25 women out of a group of 100. Then you would need a second group of pregnant women who receive one-on-one outreach visits. Count how many of them attend antenatal care – let’s say it’s 42 women out of a group of 100. Then subtract how many attended from the first group (42-25 = 17). That means the one-on-one outreach resulted in 17 extra women attending antenatal care. You also need a third group of women who receive SMS messages reminding them to attend antenatal care. Count how many of them attended. Let’s imagine that it was 31. Subtract the number who attended in the first group (31-25=6), meaning that 6 extra women attended antenatal care as a result of receiving the SMS.
- Calculate the costs: The next step is to work out how much each activity cost. Make sure you take into account every cost associated with the activity, including the cost of the time that staff spend organizing and implementing it. Keeping with the same example, this would mean adding up all the costs for the one-on-one outreach sessions, then separately adding up all the costs for the SMS messaging. Let’s say that the total cost of the one-on-one outreach for 100 women was $3,500 and the total cost of the SMS messages was $700.
- Divide the cost by the outcome for each activity: To calculate the cost-effectiveness for each activity divide the total costs by the outcome. In this example that means dividing the total cost of one-on-one outreach or SMS messages by the total number of extra pregnant women who attended antenatal care. In this fictitious example, SMS messages are more cost effective that one-on-one outreach when it comes to getting women to attend antenatal care.
Limitations of this method
This is a very basic method for doing cost-effectiveness analysis. It is useful when you want to compare different activities that have exactly the same outcome in order to save money. However, it’s important to realize the limitations. Cost-effectiveness analysis only looks at one outcome. In this example it was the number of women attending antenatal care. It doesn’t take into consideration other factors.
For example, it’s possible that one-on-one outreach had other benefits for vulnerable women (emotional support or increased knowledge of good childcare practices) which were not provided by the SMS messages. One-on-one outreach also achieved a higher participation in antenatal care, so if you wanted the maximum number of women to attend it might still be a better choice.
There may also be times when it is difficult to accurately measure the costs or outcomes of a particular activity. This is often the case when multiple activities are integrated into one program, and there aren’t separate groups of people receiving different activities. In this case cost-effectiveness analysis may not be appropriate.
Applications of CEA[5]
Sometimes called cost utility analysis, a cost effective analysis is one performed to compare the relative costs involved in achieving identical outcomes from different activities. This method is used in a variety of different applications, including but not limited to:
- Marketing, where metrics are used in determining the long-term value of marketing initiatives. Examples include testing the conversion rates for different campaigns, customers completing purchases vs. abandoned carts, impact on long-term growth based on online versus offline initiatives, etc. Marketers are increasingly leveraging CEA to balance the value created by “upper funnel” tasks such as brand building with the hard-coin ROI from “lower funnel” tasks of converting potential buyers into paying customers.
- Purchasing, where CEA is applied to improve decision making and select goods and services that deliver optimal results. In some cases, a slightly more expensive option may provide substantially greater performance, longevity, sustainability, etc. and therefore be a more valuable and intelligent purchase despite its higher relative cost. The most effective purchase is one that considers the immediate and the long-term, as well as the concrete (e.g., profitability) and the intangible (long-term value from more sustainable materials, greater market share due to the use of those materials, etc.).
- Health and medicine, where CEA helps inform health policy, provide payers with maximum value through lower TCO and higher ROI, and ensure effective asset allocation for different health services. The World Health Organization (WHO) has been engaging in CEA since the late ’90s. Its WHO-CHOICE program seeks to help governments and organizations leverage digital platforms to conduct systematic reviews of potential activities and optimize the efficacy of different health interventions in promoting a healthy life. In the health services arena, CEA can include economic evaluation of different interventions, but it looks beyond monetary value. It also considers the health benefits of clinical trials, the efficacy of different health care interventions as compared to taking no action, and the impact of different health interventions and their outcomes (i.e., associated health effects) on quality of life (as measured in quality-adjusted life years (QALY)) over the patient’s total years of life remaining.
A more advanced example of a CEA metric being used in health economics is incremental cost-effectiveness ratio (ICER). This metric is used to evaluate the change in relative costs and “units of health” as the effects of a given health care intervention change. Generally, this concerns how many additional life years (i.e., QALYs) are created based on additional spend.
- Energy efficiency studies, where “negawatts” express the energy that is not consumed due to investment in energy efficient technologies or practices.
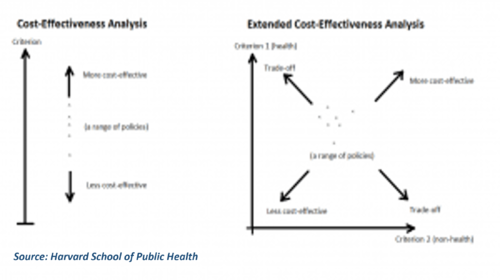
Extended Cost-Effectiveness Analysis (ECEA)[6]
Extended Cost-Effectiveness Analysis (ECEA) is a form of quantitative economic analysis that assesses the health and financial impact of health policies. It is an expansion of cost-effectiveness analysis, which compares the relative costs and gains in health outcomes (in the form of years of life saved, premature deaths averted, quality- or disability-adjusted life years gained/averted, etc.) of interventions. ECEA also includes non-health benefits such as financial risk protection and distributional consequences like equity in the economic evaluation of health policies. This enables health policy makers to take into account multiple criteria and make trade-offs among competing demands (see Figure below).
Benefits and Drawbacks of Cost-Effective Analysis[7]
Benefits of Cost-Effective Analysis Cost-effective analysis can be extremely beneficial when comparing interventions with one another, in particular when researchers want to:
- Compare different programs for the same disease
- Compare different programs for a certain demographic sector
- Compare different interventions for different diseases
The cost-effectiveness calculation is particularly useful when relating different programs that are focusing on the same disease or goal. However, it is also advantageous when looking at interventions that address differing diseases and risk factors. When resources are limited, it is critical that they are used in the most cost-effective interventions possible. For example, imagine that you have one million dollars and two options on how to spend it: you can either invest the money to increase Hib vaccinations for children and save 10 – 800 lives, or invest the same amount to increase measles vaccinations for children and save 800 – 66,000 lives. Cost-effective analysis highlights that the second option is the best allocation of resources: if the number of lives saved is the measure of health gain in the analysis calculation, then the best intervention is the one that averts the most deaths.
In order to use information about cost-effectiveness of past interventions in the most valuable way possible, it is important to:
- Take into account how prices, demographics, epidemiology or service coverage would differ substantially in the specific region
- Consider whether or not this intervention targets the chief causes of disease in the country
- Decide if the interventions are practical based on standing establishments and past experiences
- Assess the cost-effectiveness considering how the intervention is implemented and how items are distributed
Reviewing evidence in this way will tremendously assist countries and organizations to improve individuals’ health, as the expenses and results of the different options will be clearly demonstrated.
Limitations and Drawbacks of Cost Effective Analysis
There are, however, drawbacks to cost effective analysis. Organizations often differ in their ways of performing the calculation. Some studies place the same value on every life regardless of age (i.e., an infant and a middle-aged adult are weighted equally), whereas other studies take into account how many years an individual has left to live (i.e., stopping infant diarrhea is considered largely more successful than rescuing someone older from stroke). Prices also greatly influence cost estimates, which can differ substantially even within a single country. Analysis also depends on the scope of the costs (narrow versus broad definition of “cost”), and additional costs that the researcher has selected to take into account, such as dedication of time and transportation value. Differences in choices of these measurement units significantly impact the interpretation of the analyzed information.
Challenges to Conducting CEA
It is no secret that conducting a Cost-Effectiveness Analysis (CEA) can be difficult. In fact, many challenges exist when trying to measure the cost of an intervention and its impact on a single outcome. For one, it can be hard to obtain accurate cost estimates from other sources. This is due in part to exchange rates, inflation rates, and discount rates- which make comparisons between studies or programs difficult.
Another challenge faced when conducting CEA is that they often take a long time to complete. Aggregating across multiple outcomes also proves to be difficult- especially when trying to measure costs over different time periods.
Despite these challenges, there are some considerations for how to calculate costs that researchers must take into account. These include research methods, economic assumptions, and what impacts you want to measure/costs over which time periods/etc..
One exception where CEA has been used in the past is with "National recommendations on immunization policy." The Centers for Disease Control and Prevention's Advisory Committee on Immunization Practices uses Cost-Effectiveness Analysis as a tool when making national recommendations about immunizations.
However, using CEA evidence for health care decisions is not uncontroversial in America. Many people are resistant to the idea of accepting limits on the delivery of health care. This may be partly due to a lack of understanding about what rationing would entail and how it would affect them personally. However, conducting CEA remains an important tool in assessing the value of health technology. Methods have been improved over time, but there is still room for growth in this area.
Ethical Considerations for CEA[8]
There have been a few criticisms on ethical grounds of CEA’s use for decision making. These include:
- Controversies associated with the use of QALYs: The lower health utility, or health-related quality of life, assigned to patients with worse health (because of more severe disease, disability, age, and so on) raises distributional issues in using QALYs for resource allocation decisions. For example, because patients with disabilities have a lower overall health utility weight, any extension of their lives by reducing the health burden from one disease “would not generate as many QALYs as a similar extension of life for otherwise healthy people.” This distributional limitation arises because of the multiplicative nature of QALYs, which are a product of life-years and health utility weight. Consequently, the National Council on Disability has strongly denounced the use of QALYs. Alternatives to QALYs have been proposed. The Institute for Clinical and Economic Review has started using the equal value of life-years gained metric, a modified version of the equal value of life (EVL) metric, to supplement QALYs. In EVL calculations, any life-year gained is valued at a weight of 1 QALY, irrespective of individuals’ health status during the extra year. EVL, however, “has had limited traction among academics and decision-making bodies” because it undervalues interventions that extend life-years by the same amount as other interventions but that substantially improve quality of life.30 More recently, a health-years-in-total metric was proposed to overcome the limitations of both QALYs and EVL, but more work is needed to fully understand its theoretical foundations.
- Distributive justice. The second criticism pertains to the fundamental notion that “a QALY is a QALY is a QALY no matter who gets it.” Because of this egalitarian notion, the question of whose values shall count for how much raises some ethical issues. For example, should large benefits to a small number of people receive priority over smaller but greater aggregate benefits to a large number of people? Or when should society give priority to treating the sickest or worst off? However, CEA was not meant to address such distributional considerations directly. The Second Panel on Cost-Effectiveness in Health and Medicine emphasized that such distributive considerations also matter to decision makers and are often part of deliberative processes. Areas of ongoing research include the development of equity weights, which assign numerical values based on considerations other than QALYs (eg, the severity or rarity of the disease), and incorporating social distributions of health (eg, by income or ethnicity) into CEA.
- Incomplete valuation. The third criticism relates to CEA’s consideration (or lack thereof) of certain value elements. Many HTA bodies around the world use CEA from a health care sector perspective and do not incorporate value elements such as productivity, time costs, caregivers’ costs, and spillover to other sectors of the society. Even in the United States, ICER has not considered these elements formally, although more recently it has allowed for a modified societal perspective as a secondary analysis.7 The Second Panel on Cost-Effectiveness in Health and Medicine, which recommends analyses using both the health care sector perspective and the societal perspective, has laid out the methods for incorporating such value elements. Often, lack of data (eg, the effect of a treatment on productive time) precludes analysts from including some of these value elements in the analysis, even though they are generally believed to be important to patients and their caregivers. Although recent advances in measuring these value elements have provided a set of useful resources, more work is needed to readily incorporate these elements into standard CEA.
While the criticisms have been discussed in detail here, it is worth pointing out that cost-effectiveness evidence is only one of many factors considered in resource allocation decisions. It has been found that none of the international HTA bodies bases its decisions solely on cost-effectiveness evidence. Therefore, much of CEA’s criticisms, fair or not, can be addressed through deliberative processes.
See Also
References
- ↑ Understanding Cost Effectiveness Analysis (CEA) MSR
- ↑ Explaining Cost Effectiveness Analysis (CEA) BetterEvaluation
- ↑ Considerations for cost calculations World Bank
- ↑ How to do a basic cost-effectiveness analysis Tools4dev
- ↑ Applications of CEA Planergy
- ↑ What is Extended Cost-Effectiveness Analysis (ECEA)? HSPH
- ↑ Benefits and Drawbacks of Cost-Effective Analysis Unite for Sight
- ↑ Ethical Considerations for CEA David D. Kim, PhD and Anirban Basu, PhD